Abstract

Background:
Women with sickle cell disease (SCD) are at high risk for obstetrical and SCD-related complications throughout pregnancy. Given the dearth of recent population-based studies on female reproductive health in SCD, we used hospitalization data from the socio-economically diverse state of California to describe peripartum outcomes in women with SCD.
Methods:
For our retrospective cohort study, we identified females with SCD who were either evaluated in the emergency department (ED) or hospitalized between the ages of 10-45 years from California's patient discharge dataset (1991-2016). We defined SCD severity by frequency of utilization with severe disease requiring an average of ≥ 3 hospitalizations and/or ED visits per year, and less severe with an annual rate of < 3 acute care visits. We used ICD-9/10-CM codes to identify all deliveries, and categorized pregnancy outcomes as either incomplete (hydatidiform mole, elective termination, miscarriage, and ectopic pregnancies) or delivery (live or stillbirths). We defined race/ethnicity as Black (or African American) vs. non-Black and quantified the total number of pregnancies for each patient. We described delivery age, mode (C-section vs. vaginal), outcome (live vs. stillbirth), median length of stay (LOS), and maternal mortality for the first in-hospital delivery.
Results:
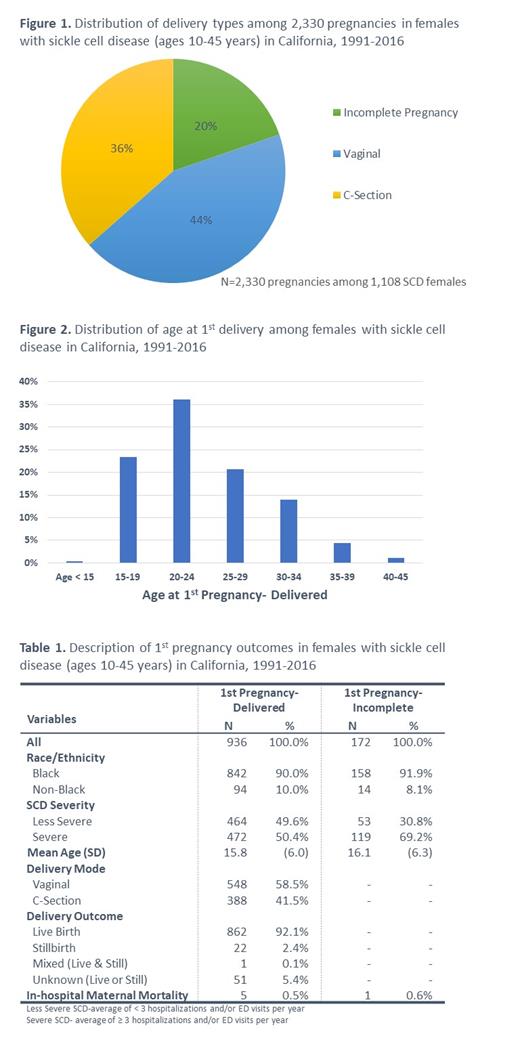
Our cohort comprised 3,089 females with SCD of childbearing age, with a median follow-up of 11 years. Of the 1,108 (35.9%) women with at least one pregnancy, 1,000 (90.3%) were Black and 591 (53.3%) had severe SCD. Overall, we observed 2,330 pregnancies; of the 1,864 (80%) deliveries , 45% occurred via C-section (Figure 1). When we restricted our analysis to first deliveries only, 346 (36.0%) occurred in women ages 20-24 years; the next highest proportion of deliveries (23.4%) was in adolescents ages 15-19 years (Figure 2). Only 5.5% of deliveries occurred in women ≥ 35 years old. One hundred seventy-two (15.5%) first pregnancies were incomplete (Table 1), primarily due to miscarriage (59.3%). Of the women with incomplete first pregnancies, 69.2% had severe SCD; in contrast, 50.4% had severe SCD in the first delivered pregnancies' subset. Of the 936 first deliveries, 41.5% were by C-section with a median LOS of 5 days, compared with 3 days for those who delivered vaginally. Twenty-two first deliveries (2.4%) were stillbirth for a rate of 24.9 stillbirths per 1000 deliveries. Of the 862 live births, 5 women died, which resulted in an inpatient maternal mortality rate of 580.1 per 100,000 live births.
Discussion
Pregnant women with SCD first delivered in the hospital at a mean age of 24.1 years, which is younger than the US national mean of 26.8 years (all races) and 24.9 years (Black), based on 2017 maternal health data from the Centers for Disease Control and Prevention (CDC). We attribute this age difference to the higher proportion of first deliveries in adolescents with SCD coupled with the trend towards older age of first delivery in the general population. For first deliveries, 41.5% of women with SCD underwent a C-section, compared with a 2013 national average of 22.8% (all races) and 25.7% (Black) in primigravid women in the US. Stillbirths in our SCD cohort surpassed the 2014 national rates of 5.9 (all races) and 10.3 (Black) stillbirths per 1000 deliveries. Lastly, the inpatient maternal mortality rate in women with SCD, while based only on 5 deaths, far exceeds the 2014-2017 US maternal mortality rates of 17.3 (all races) and 41.7 (Black) deaths per 100,000 live births.
Limitations include the lack of outpatient data, which likely resulted in an underestimation of the total number of pregnancies. Maternal mortality rates from the CDC cover death up to 12 months postpartum, so a comparable mortality rate for women with SCD might be higher. The striking disparities in outcomes in our study cohort, compared to national averages, suggests notable deficits in the optimal management of pregnancy in SCD. Analyses are ongoing to determine the effect of pregnancy on sickle-cell related complications, to evaluate the frequency of peripartum complications in women with SCD (e.g., venous thromboembolism, preeclampsia, and post-partum hemorrhage), and to compare rates of obstetrical complications in SCD vs non-SCD women, adjusted for social determinants of health.
No relevant conflicts of interest to declare.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract